A new gene-editing technique may be capable of fixing almost all disease-causing genetic defects — with fewer off-target effects. The new CRISPR gene-editing technique, described in a Nature paper published on 21 October, can be used to edit human cells more precisely and efficiently than ever before, thereby expanding the possibilities of gene editing (1).
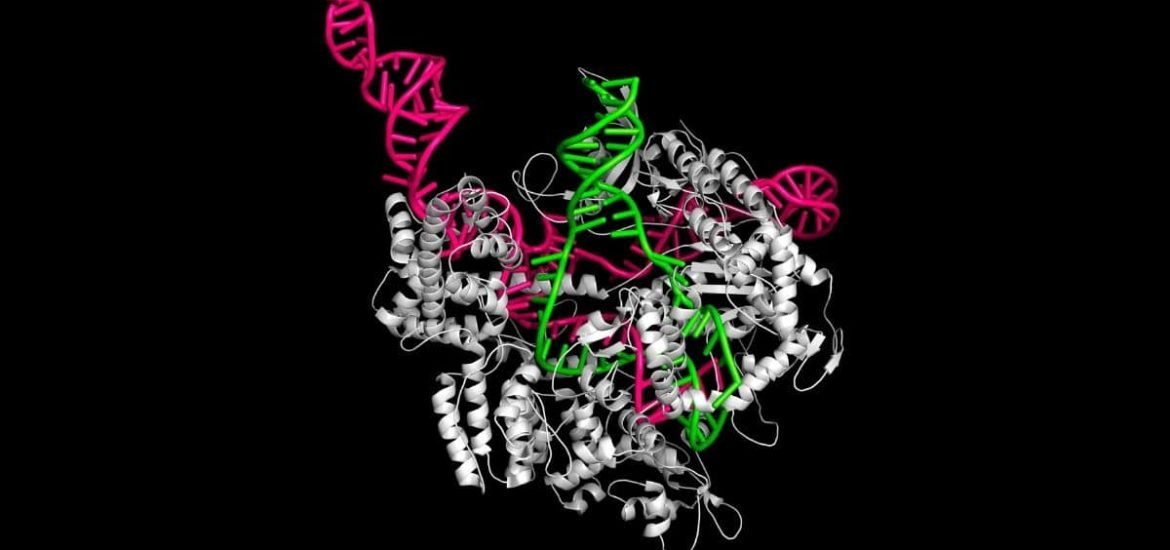
The so-called “prime editing” system works by combining two proteins — CRISPR-Cas9 and reverse transcriptase — and a single RNA into a single system. This gives researchers far more control over the DNA changes that are made and brings scientists one step closer to the ultimate goal of making prices changes to the genome at any location.
The new system has the ability to correct up to 89 per cent of “point” genetic mutations, the authors claim. Point mutations are changes to a single nucleotide base in a sequence of DNA or RNA and are responsible for diseases like cystic fibrosis, sickle cell anaemia, Tay-Sachs disease, and phenylketonuria. According to ClinVar, a public database maintained by the National Center for Biotechnology Information (NCBI), there are around 75,000 known disease-associated DNA variants.
The very first CRISPR approach uses the protein Cas9 to completely cut DNA sequences, then certain segments of DNA are inserted or deleted with the hopes of effectively fixing the genetic disease. But using these so-called molecular scissors to make double-stranded breaks in DNA can lead to unintentional modifications to of genetic material, which could potentially activate other cancer-causing genes.
Another approach called base editing allows precise editing of DNA by chemically converting one DNA letter directly into another without the need for double-stranded breaks — and although more precise, is limited to four out of 12 types point mutations. Now, an alternative approach that does not require double-stranded breaks has been developed and can correct all 12 types of point mutations.
By combining Cas9 with another protein called reverse transcriptase, the researchers have found a way to use RNA to direct the insertion of new DNA sequences into human cells. Much like the traditional CRISPR-Cas9 system, the Cas9 enzyme is still used. But in this case, it only cuts a single DNA strand. Then, another enzyme called reverse transcriptase is guided by the single strand of RNA to make the appropriate modifications at the site of the cut.
The new CRISPR gene-editing technique was successfully used to correct the genetic defects that cause sickle cell disease and Tay-Sachs disease in humans cells in the laboratory, the authors report.
The new approach reduces the risk of unwanted changes or off-target effects, which has been a key challenge when applying the standard CRISPR–Cas9 system. Therefore, prime editing could potentially make gene editing much safer — but requires a lot more testing before clinical use.
“We’re not aware of another editing technology in mammalian cells that offers this level of versatility and precision with so few byproducts”, says senior author Prof David Liu. Moreover, the new tool will also make it easier to develop disease models in the laboratory and to study the function of specific genes, Lui told Nature.
While prime editing is unlikely to replace the CRISPR-Cas9 system completely — since it cannot make the same large insertions and deletions that CRISPR-Cas9 is capable of — scientists believe a range of gene-editing platforms will be needed in the future. And thus far, prime editing seems to be the most precise and versatile.
(1) Anzalone A.V., et al. Search-and-replace genome editing without double-strand breaks or donor DNA. Nature (2019). DOI: 10.1038/s41586-019-1711-4