
In an earlier article, we saw that the prospective epidemiological studies on the health of farmers (AHS cohort in the USA, Agrican cohort in France), supposedly the most reliable ones, gave very reassuring results overall for the vast majority of cancers: only 3 types of cancer showed greater incidences than normal, and no abnormal mortality was observed. However, the mechanisms of the research made it such that these reassuring results were not analyzed in sufficient depth by the epidemiologists in order to say that there is no risk, as the precautionary principle requires. The health agencies, whose job it is anyway, would therefore need to perform additional analyses for this purpose rather than simply summarize the results of scientific publications, which by nature focus on the rare significant results suggesting a risk.
We will now look at the three types of cancer (lip cancer, prostate cancer, multiple myeloma) for which these prospective studies all agree that there is a significantly excessive rate of incidence among farmers. None of these three types of cancer is currently classified as an occupational disease of farmers in France. However, the Agrican cohort stakeholders are advocating the rapid listing of the last two types as such. Although this makes sense, we shall see that there are still some questions regarding these two diseases that remain to be answered unless we want to end up in the same impasse as with non-Hodgkin’s lymphoma (NHL): in 2015, this type of cancer was classified as an occupational disease of farmers exposed to pesticides. But three years after this classification, INSERM (French National Institute of Health and Medical Research) stated that it could not quantify the number of victims potentially entitled to compensation… or even show that there really were cases of excessive rates of incidence among farmers[1].
Lip cancer: not a good subject?
Curiously, lip cancer is by far the form with the most excessive rate of incidence among farmers… but also the one that is least discussed! The incidence of lip cancer among farmers who use pesticides is nearly double that of the general population, both in France and in the USA (at least in North Carolina):
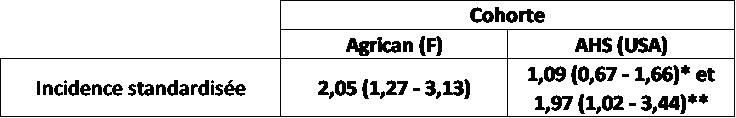
Table 1: Standardized incidences (mean and 95% confidence interval) of lip cancer among farmers using pesticides in the two largest prospective cohorts of farmers: Agrican (France) and AHS (USA: * Iowa ** North Carolina). Example of interpretation: there is a significant excess of 97% (Standardized incidence = 1.97) in the AHS cohort in North Carolina.
In our previous article, we saw repeatedly that for many cancers, the standardized mortality rates were distinctly lower than the standardized incidences. Is this the case for lip cancer? Impossible to say: as far as mortality was concerned, lip cancer was grouped with the other oral cavity (mouth and pharynx) cancers in both the Agrican and AHS cohorts. As these cancers are mainly caused by tobacco and since farmers smoke less than the general population, their mortality rate for all of these oral cancers is much lower (-66% in the USA, -49% in France, significant in both cases) than average, which masks the probable excessive mortality due to lip cancer. Why this grouping with cancers of the oral cavity, which makes no sense from an epidemiological standpoint? We fear that this is yet another example of how scientific publications tend to gravitate toward statistically significant results: the deaths are very fortunately far less numerous than the cases of cancer. Consequently, there is clearly more uncertainty over the mortality rates than over the incidence rates… and in both cohorts, the publications on mortality grouped related diseases in order to increases their chances of obtaining significant results. It was in this manner that the mortality rate of the type of cancer with the most excessive incidence rate among farmers and, more generally, the inconsistencies between incidence and mortality, were obscured. However, we shall see that regarding prostate cancer, these inconsistencies are a true scientific subject that deserves further study.
For lack of results on mortality, the incidences of lip cancer among farmers should suffice to make it a priority health alert. Why is this not the case? Here we touch on the main bias in the interpretation of these cohort studies: they are clearly conducted to identify pesticide effects rather than to investigate the health problems specific to farmers in a neutral manner. The excessive incidence rate of lip cancer is a phenomenon that has already been observed in other outdoor occupations such as road workers or fishermen. It is generally attributed to exposure to the sun, hence it is not a “good” subject for Agrican… The result: No communication for the prevention of this cancer among farmers, even though it would be easily avoidable with a minimum awareness-raising effort.
Prostate cancer: very consistent results, but clarification required
There has been much more communication regarding prostate cancer, to the point that the Agrican team is taking steps to have it classified as an occupational disease associated with exposure to pesticides. P. Lebailly, the coordinator of the cohort, recently explained: “There is clearly no scientific reason why prostate cancer linked to the use of plant protection products should not be included in a table [of agriculture-related occupational diseases]”[2]. There is certainly some basis for this, since the excessive incidence among farmers is significant and very close (ca. +20%) in both large cohorts. However, some additional studies might be useful given the fact that the results on mortality of the two cohorts are just as consistent… but show the opposite trend!
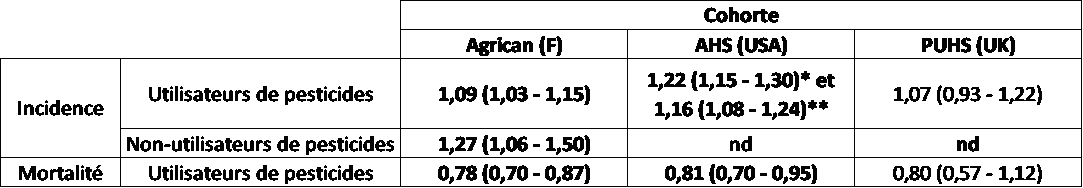
Table 2: standardized incidence and mortality rates of prostate cancer in the main prospective cohorts on the health of farmers[3]. The results are very consistent: every time an excess incidence was clearly observed in farmers who use pesticides…as was a mortality rate lower than in the general population! Results that may be explained not only by better health in farmers, but also by earlier detection in them, which should come as no surprise in view of the suspicions expressed regarding this disease for sometime. Furthermore, the excessive incidence rate is just as high (if not higher) among farmers who do not use pesticides. Thus some additional studies are evidently needed before classifying prostate cancer as an occupational disease of farmers… and above all for demonstrating a link between it and exposure to pesticides!
The mortality rate among farmers due to this cancer is in fact significantly lower (20% in both cohorts) than that of the general population. The exact same trends can be observed in the British cohort PUHS (the results are not significant due to the smaller sample size of this cohort and its shorter follow-up period, but they definitely show the same trend). This inconsistency between incidence and mortality, surprising yet statistically confirmed, should have long since prompted specific studies for determining the causes. Indeed, it implies that the prognosis for prostate cancer diagnosed in farmers is better than that for the rest of the population. This could be due to the well-known “healthy worker” effect already mentioned in our previous article, but which as we have already seen is hard to demonstrate in Agrican. But there is another equally plausible explanation, especially for this cancer, for which screening plays a major role in detection: in the general population it has been shown that thanks in part to earlier screening, the prognosis for prostate cancer has greatly improved over the last twenty years[i]. Given that there have been recurring suspicions of excessive rates of prostate cancer in farmers for 20 years, it should come as no surprise that farmers are more willing to undergo screening than the general population (and that MSA [French agricultural social insurance] doctors urge them to do so). This could explain both the apparently higher standardized incidence and the lower standardized mortality that was observed in the two cohort studies. This hypothesis, entirely plausible, could be verified according to the method that INVS [French Institute for Public Health Surveillance] used in its previously cited study: by comparing the average clinical stages at detection of the disease, among farmers and in the general population. We are sure that the Agrican team has the wisdom to perform this verification before having this cancer listed in the table of occupational diseases…if for no other reason than to anticipate the number of potential victims!
If this verification confirms that there truly is an excessive rate of prostate cancer among farmers, there will be one more step to take for classifying it as a disease caused by exposure to pesticides. Some results from the AHS cohort admittedly suggest a positive association with certain organochlorine and organophosphate insecticides[4]. But thus far the Agrican data are not showing that this is necessarily true: the last assessment of incidences in the Agrican cohort admittedly revealed a significant excess of prostate cancer among farmers (+9%)… but the excess is even higher among non-users of pesticides! (+27%, a result that is admittedly not significantly different from that for pesticide users, but significantly greater than that for the general population). According to INSERM, this would be explained (seriously) by the “role of diverse risks such as an indirect or secondary exposure to pesticides applied to the crops or animals, and while handling grain or hay”… This reasoning is reminiscent of a well-known trick: “Heads I win, tails you lose”: when an incidence higher than 1 is found among pesticide users, this proves that pesticides cause cancer; when it is found among non-users of pesticides, this shows that they were contaminated by the pesticides in a hidden fashion… This is admittedly a possible explanation, but frankly not the simplest one! Even less so since this “disturbing” result is not isolated: an American meta-analysis, focusing this time on case-control studies of prostate cancer, found a significant but negative link with exposure to pesticides[5]. According to this meta-analysis, the risk of prostate cancer is significantly reduced by 32% in farmers who use pesticides compared to those who do not use them. The statistical significance of this meta-analysis must admittedly be viewed with caution, since it only included 4 studies with rather small sample sizes. But at any rate, it shows that affirming that pesticides alone are responsible for the excessive rates of incidence of this cancer among farmers, even in the case-control studies that are the main “witnesses for the prosecution” in the pesticide proceedings, is a bit of a stretch.
The case of multiple myeloma and non-Hodgkin’s lymphomas
According to the prospective investigations, multiple myeloma (MM) logically ought to be the disease of greatest concern. Indeed, the standardized incidence of this disease is significantly higher than 1 among pesticide users in the Agrican cohort and in the AHS cohort (at least in North Carolina, but not in Iowa). Furthermore, it is one of the rare diseases in the Agrican cohort for which the standardized incidence is higher among pesticide users (+49%, significant) versus non-users (-2%, not significant). Special scientific vigilance would therefore be justified for this disease. But the Agrican data as currently presented do not make this task easy. In fact, the opposite is true.
In the case of prostate cancer, we have seen that an excessive incidence rate does not necessarily translate to an excessive mortality rate. The Agrican team did not publish the standardized mortality for this disease: in its last point on the causes of mortality in the cohort[6], multiple myeloma was grouped with all lymphatic and hematopoietic cancers, the standardized mortality of which is significantly lower (-17%) than normal. As in the case of lip cancer, this grouping is quite surprising. It is all the more regrettable that the AHS cohort results once again raise the question of consistency between incidence and mortality: the mortality rate of multiple myeloma does not show any significant excess (+1%, NS), whereas the incidence results were contradictory (+2% NS in Iowa, + 42% significant in North Carolina). Hence it would have been worthwhile to have the mortality of multiple myeloma in Agrican for a clearer picture.
This amalgam of multiple myeloma and NHL was likewise made without more epidemiological justification in the recent Agrican publications on incidences. This makes it impossible to distinguish the case of non-Hodgkin’s lymphoma (NHL), which is classified as an occupational disease of farmers, from the case of multiple myeloma, which is not, even though the epidemiological results of the latter are objectively much more disturbing than those of NHL. In an earlier article[7], we already saw that this ambiguity probably led the interdepartmental mission on compensation for pesticide victims to count the victims of multiple myeloma twice in error. But it gets even more bothersome: this grouping of myelomas and NHL makes it impossible to judge the relevance of the classification of NHL as an occupational disease caused by pesticides. Clearly there are issues regarding this subject that need to be addressed:
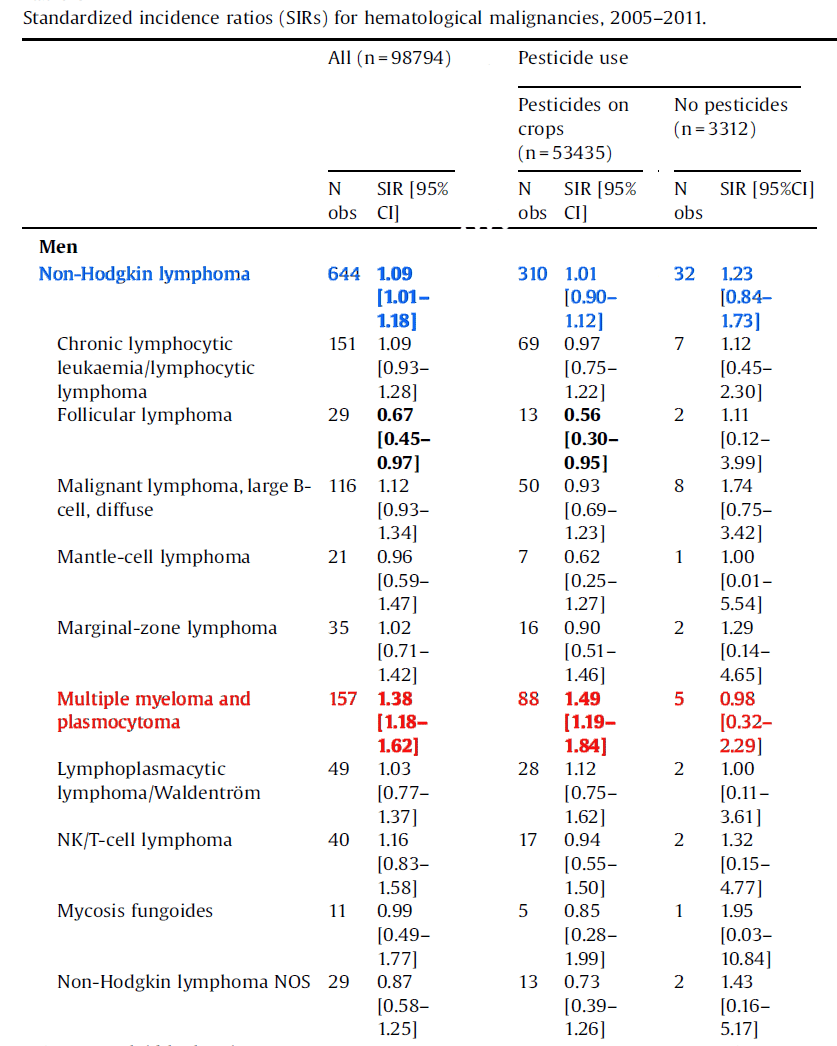
Table 3: Incidence of non-Hodgkin’s lymphomas (NHL) in the Agrican cohort (excerpted from table 6 of Lemarchand et al 2017). A significant excess of 9% (SIR = 1.09) of NHL among farmers as a whole can be observed (line in blue). But the incidence among farmers who use pesticides on crops is perfectly normal. This excess is mainly seen in non-pesticide users (+23%, not statistically significant). More importantly, this is in fact a cumulative result of NHL and multiple myeloma (MM). The latter is a similar type of cancer, but unlike NHL it is not classified as an occupational disease. The results of this grouping is heavily affected by MM, because it accounts for 162 cases of the 676 registered, and the results for it are contrary to the general trend (it is the only disease for which the incidence among pesticide users is considerably higher than that among non-users). If we were to remove MM from this grouping, it is likely that the incidence of “true” NHL among pesticide users would be lower than that of the general population. This is what was observed in the AHS cohort, in which the American researchers were careful not to mix the multiple “apple” with the non-Hodgkin’s “oranges”. In contrast, the incidence among non-users of pesticides would remain considerably higher than 1. This would raise some hard questions regarding the relevance of classifying NHL (excluding MM) as an occupational disease caused by pesticides…
The standardized incidence of “true” NHL (excluding multiple myeloma) cannot be recalculated from the results published by INSERM[8]. However, a simple examination of the Agrican figures (Tab. 3) shows that, if MM were excluded:
- for farmers who use pesticides, the standardized incidence of NHL would be distinctly lower than that of the general population
- but for farmers who do not use pesticides, it would remain substantially higher than 1
In light of these results, we understand more clearly the difficulties faced by INSERM when asked to estimate the number of cases of NHL caused by pesticides… This estimate can only be made on the basis of prospective epidemiological studies, none of which shows an excessive rate of NHL among farmers who use pesticides: neither relative to the general population nor relative to farmers who do not use pesticides!
In spite of all of this, why was NHL classified as an occupational disease caused by pesticides? We have just seen that there is no observable excessive rate of NHL among farmers who use pesticides as a whole. This does not mean that certain specific pesticides could not cause NHL, but it does mean that this effect does not appear in the statistics in the case of products used by few farmers. NHL is one of the cancers for which dose-response relationships have been observed, namely between exposure to certain products and the risk of getting cancer. IARC (the International Agency for Research on Cancer) published a meta-analysis on this subject in 2014[9]. It undoubtedly inspired those who included NHL in table 59 of agriculture-related occupational diseases[10], because this table explicitly lists the products highlighted by this meta-analysis: organochlorine and organophosphate insecticides, carbaryl, toxaphene, and atrazine. Unfortunately, this meta-analysis places the same importance on case-control studies (the most numerous) and prospective studies (more reliable, but much less numerous). And, in the majority of cases in which a prospective study was performed on a molecule, that study did not reveal the effect suggested by the case-control studies (for example, this is the case with atrazine, carbaryl, most organophosphate insecticides, …and glyphosate, which is the source of much controversy today). This IARC meta-analysis is thus based on methods questioned by all health authorities, as we have seen in the example of glyphosate. Using it as a basis for establishing the list of products likely to cause NHL is thus rather risky, and once again it makes it impossible to quantify the number of potential victims, since the data only come from case-control studies.
Is a reconsideration necessary?
In the first part of this article, we saw that the first concerns about cancer among farmers came from so-called case-control epidemiological studies, which suggested excessive incidences of cancer among farmers but were unable to put figures on them. So-called prospective epidemiological studies, which are reputedly more reliable, were then initiated for quantifying the number of victims. To date, they clearly show that the risk of cancer among farmers is lower or equal to that of the general population (with the possible exception of multiple myeloma), contrary to what the case-control studies would have us believe. The only remaining doubt about this subject is the possible existence of a “healthy worker” effect that would mask the carcinogenic effect of pesticides. However, epidemiologists have not provided any proof of the existence of this effect thus far. Pending this proof, there is no reason to suppose that farmers as a whole are vulnerable to cancers caused by their exposure to pesticides. Furthermore, the French prospective cohort Agrican, the only one permitting this question to be studied, does not show any significant excessive rate of cancer among farmers who use pesticides relative to those who do not.
It is obviously possible (even most likely) that only certain pesticides have carcinogenic effects at the concentrations to which farmers are exposed. This would explain why these harmful effects are not perceivable among farmers on a global scale. Many scientific publications claim to have identified a dose-response relationship between exposure to certain pesticide molecules and certain cancers and therefore reinforce this view. However, as we have seen in the example of the IARC meta-analysis of non-Hodgkin’s lymphoma, these results come almost exclusively from case-control studies and as a general rule they are not confirmed in prospective studies.
In view of these persisting discrepancies between case-control and prospective studies, an agreement on the level of proof required for classifying a product as hazardous would need to be reached. This was what the debate on glyphosate between IARC (which classified it as a probable carcinogen based on 4 case-control studies, whereas the 5 available prospective studies on the same subject did not show any effect) and all of the health authorities that refuted the IARC classification boiled down to. In terms of sanitary expertise, this question is essential for two reasons:
- In order to avoid impasses such as those encountered by the pesticide victim compensation fund in the case of non-Hodgkin’s lymphoma, prospective results would be needed in order to quantify the number of potential victims of diseases classified as occupational. Moreover, the examination of results from prospective cohorts raises new questions: what standard of reference must be used for establishing the occupational nature of a disease? The general population? Farmers who do not use pesticides?
- At this point, the results from prospective cohorts are sufficiently accurate and consistent for estimating the differences in mortality rate between farmers and the general population. For example, it is known that relative to the general population, their mortality rate is reduced by ca. one third for cardiovascular diseases and by one half for respiratory cancers. Such differences are clearly great enough to cause statistical biases in case-control studies. It is therefore high time to use the results of these prospective studies to verify to what extent certain results of case-control studies could be statistical artefacts caused by the lower incidence among farmers of leading causes of early death.
The non-Hodgkin’s lymphoma example shows that classification as an occupational disease solely on the basis of case-control studies does not permit a clear definition of the scope of potential victims. We saw that the uncertainties about this subject are even greater for prostate cancer, where the prospective cohorts questioned not only the reality of the excessive incidence rate observed, but also the link thereof to exposure to pesticides. Let us hope that these questions will be answered (and it remains to be seen by whom, because they were not part of the work agenda recommended by INSERM) before any new classification of a type of cancer as an occupational disease. Otherwise we fear that the premature classification of certain diseases will lead to extensive litigation (as is already the case with non-Hodgkin’s lymphoma), which will only discredit the entire pesticide evaluation scheme.
[1] http://agriculture.gouv.fr/telecharger/89861?token=32f9951a0796a25966ff306e1d88e7ea
[3] References:
- Incidence rates:
Koutros et al. / J Occup Environ Med. 2010 November ; 52(11): 1098–1105 (pesticide operators/applicators; 1st figure: Iowa ; 2nd figure: North Carolina)
- Lemarchand et al. / Cancer Epidemiology 49 (2017) 175–185 (men using pesticides)
- Mortality:
Waggoner et al., Am J Epidemiol 2011;173:71–83 (men applying pesticides)
Lévêque-Morlais et al. 2014 : Int Arch Occup Environ Health DOI 10.1007/s00420-014-0933-x
[4] http://invs.santepubliquefrance.fr/beh/2016/39-40/2016_39-40_1.html
[5] Koutros et al., Am J Epidemiol. 2013;177(1):59–74
[6] Ragin et al., Am J Mens Health. 2013 March ; 7(2): 102–109
[9] C. Lemarchand et al. / Cancer Epidemiology 49 (2017) 175–185
[10] Schinasi et Léon, Int. J. Environ. Res. Public Health 2014, 11, 4449-4527;
This post is also available in: FR (FR)
Merci également pour cette deuxième partie, aussi passionnante que la première ! C’est un travail remarquable !